Needs, Outcomes, and Goals
Overview
The Needs, Outcomes, and Goals are made based on the participant’s services and their personal goals. There must be a Need, Outcome, and Goal for each service (except Service Coordination*) until you run out of available Needs/Outcomes/Goals in the “Person Centered Care Plan and Outcomes” section of the PCSP in Function Portal. If you have a N/G/O for each service and there is additional room, then the participants personal goals should be listed.
Needs
Details why the participant Needs the service or what they need help with specifically requiring the service. Always ask the participant “Why do you need this service?” or “what does this service help you with?”
- When documenting needs in the PCSP in Function portal, select the most appropriate option that matches the participants need
If there is no need that matches, select “Participant needs something else” and then specify the need in the following format like the above Example.
Examples of Needs for common services:
PAS
Why does the participant need a caregiver/what is the caregiver going to help them with?
- Ms. Amcord needs to eat diabetic appropriate meals to prevent hospitalizations for high glucose levels
- Ms. Amcord needs to take her medications as prescribed
- Ms. Amcord needs to improve mobility
- Ms. Amcord needs to improve personal hygiene
- Ms. Amcord needs to decrease hospitalizations related to falls that take place while completing bathing, dressing, and ambulation
PERS
Why does the participant need a PERS unit/what will the device do for them?
- Ms. Amcord needs to be able to access EMS and is unable to dial a phone
- Ms. Amcord needs to be able to attain assistance from EMS should a fall/injury take place
HDM
Why does the participant need home delivered meals/what will the meals provide them?
- Ms. Amcord needs to better manage her health through diet and nutrition
- Ms. Amcord needs to better manage her diet and food portion intake
- Ms. Amcord needs to have access to 2 meals per day to maintain her physical well being
- Ms. Amcord needs to prevent hospitalizations due to high glucose levels
ADC
Why does the participant need to attend ADC?
- Ms. Amcord needs to improve her socialization skills
- Ms. Amcord needs to have constant supervision and assistance with bathing, dressing, and toileting throughout each day
- Ms. Amcord needs to improve her depression and anxiety
Status of Need
Met: This indicates that the Need is already being addressed fully, through either informal, formal, or a combination of both types of assistance.
- If there is already a service in place (ie. PAS) to meet the need and there is no area of the need being unmet, then you would select “met”
- Ie. Participant has PAS provide verbal reminders during shifts to take medications, participant is taking medications 100% of the time.
Partially Met: This indicates that the Need is only partially met at the time of assistance
- If there is already a service in place (ie. PAS) to meet the need, but it is not fully met, then you would select “partially met”
- ie. Participant has PAS provide verbal reminders during shifts to take medications, but the participant is forgetting to take medications during times when PAS is not present.
- Service Coordinator should ensure a service is put into place to meet the need moving forward
Unmet: This indicates that the Need is unaddressed by either formal or informal assistance at this time.
If there is no service in place yet and the need is not met OR there is a service in place but it is not meeting the need, then you would select “unmet”.
- ie. Participant has no services yet that assist with medication reminders and is currently forgetting to take medications each day, the participant does not have family or friends to assist.
- Ie. Participant previously wanted PAS to remind them to take medications daily, but the participant wants the PAS schedule to be at times when the participant would not be taking medications. Participant is currently forgetting to take medications and does not want to move the PAS schedule.
Service Coordinator should ensure a service is put into place to meet the need moving forward
Outcomes
Details the Outcome on the participant’s life/health/well-being if the Need is satisfied.
Always ask the participant, “What are you hoping to achieve by satisfying the previously stated need?“
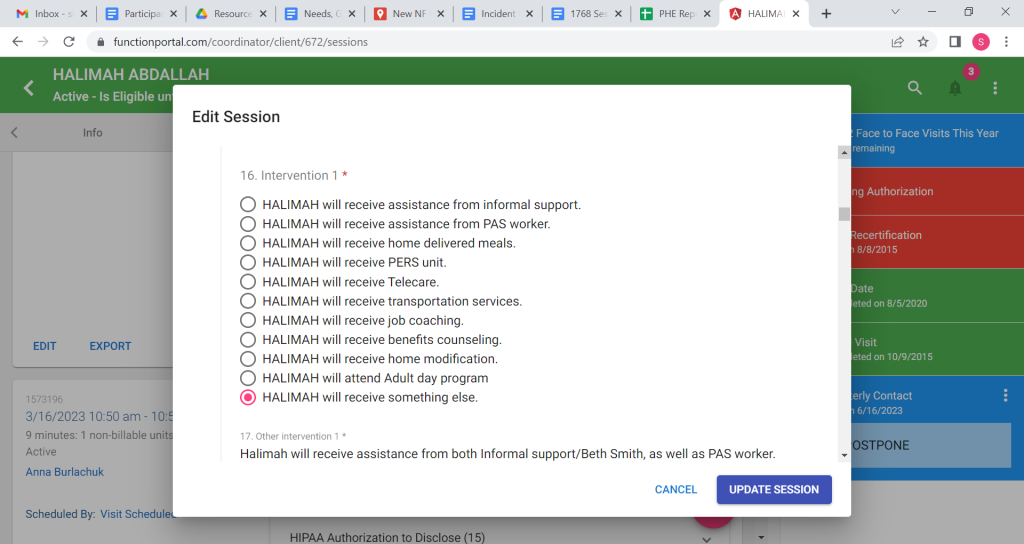
- When documenting Outcomes in the PCSP in Function portal, select the most appropriate option that matches the participants Need selection
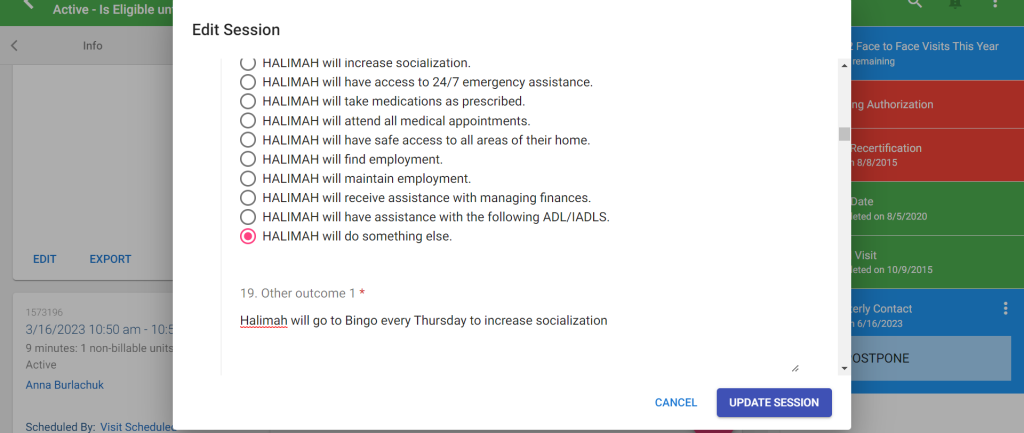
If there is no Outcome that matches, select “will do something else” and then specify the desired outcome
Goals
Details the participant’s Goal in having, receiving, or utilizing the service to satisfy the Need and obtain the desired Outcome. Goals are automatically built in SMART format, after the necessary goal related questions are answered.
1. List what diagnosis is causing the participant to experience the Need
2. Select from the list, what the goal is working towards
If no option from the list in Function Portal matches what the participant is looking for, select “other” and then write in one or two words that sum up what the participant is working towards.
3. Select from the list, who will assist the participant with meeting the goal
If no option from the list in Function Portal matches who will be helping the participant, select “other” and then write in the position of the person assisting (ie. Physical Therapist, NF staff, etc).
4. Select from list, how often the goal is being worked on
If no option from the list in Function Portal matches how often the participant will be working on the goal, select “other” and then write in the frequency that is appropriate.
Barriers
Something that prevents the participant from achieving their goals. If a participant has no informal supports this needs to be documented in the barriers. Any cognitive issues must be addressed in the barriers. There are no times where a participant does not have at least one barrier to any given goal.
- Select from the options in Function Portal, all of the barriers that the participant has related to the goal

If no option from the list in Function Portal matches how often the participant will be working on the goal, select “has another barrier” and then write in the frequency that is appropriate.
Intervention
What can/will be done to overcome the barrier and proceed with achieving the goal. If a participant has informal support they need to be listed in the interventions with the specifics of what they will be assisting with.
- Select from the list in Function Portal the appropriate response for Interventions that will be used
If no option from the list in Function Portal matches the Interventions that will be used to assist the participant, select “will receive something else” and then write in the intervention that is appropriate.


