21 Sep InterRAI
Overview of InterRAI
The InterRAI is a comprehensive person-centered review of the participant’s health and functioning, in order to properly assess their needs for services
All questions need to be reviewed with the participant and/or their responsible parties to ensure accuracy at the time of the assessment
- InterRAI is completed in Function Portal. Once you have a visit scheduled in Function Portal you will be able to document the InterRAI (ie. see alert on the right side of the screen in FP).
- All of the questions in the InterRAI must be answered.
- NEVER guess or assume answers. If you are unsure about which answer to select, ask the participant more specific questions and then select the appropriate response.
- Start with broad questions about the section
- Get more specific when needed based on the participant’s answers
- Be consistent
- There is a lot of overlap between sections of the InterRAI, and between other documents during the comprehensive needs assessment. The answers need to match between the InterRAI, PCSP, HEDIS, HRA/DSNP, and the visit session.
- There are several different sections to the InterRAI session, below are some examples of information that is covered in the assessment
- Demographic and General Information about the Participant
- Participant’s Health and Functioning (ADL/IADL’s)
- Informal supports and Formal Care
- SPG Tool: This tool is automatically populated once you have completed all prior sections
- Do NOT hit submit once completed the InterRAI, when completed you hit “add session” and select “dismiss”
Helpful Tips & Examples
Identification Information
Demographic and other general information about the participant. Much of this information can be found on the participant’s Info tab of Function Portal (this information is to be verified with the participant when doing the assessment and the information in the InterRAI and in the Info Tab must match)
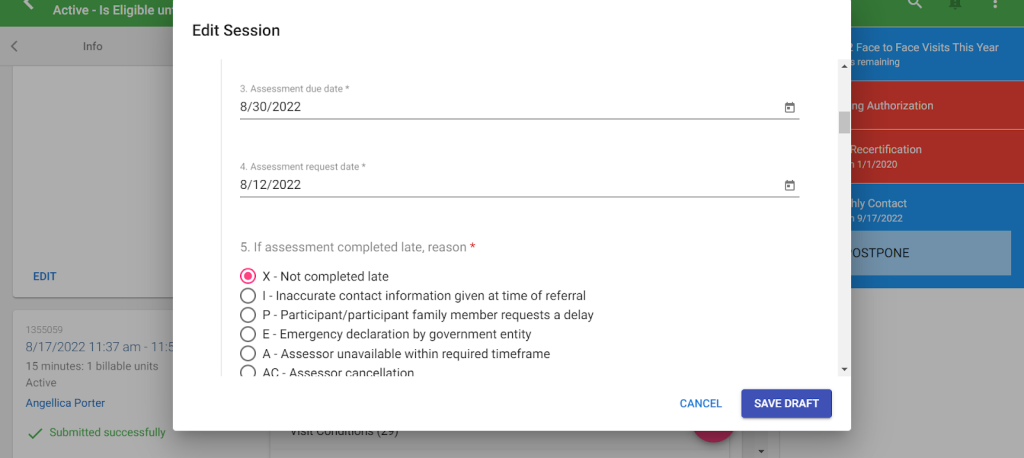
Assessment Dates
The assessment due date is either indicated in Function portal in the alerts on the right hand side of the screen (for Annual and NPO visits) or it is within 14 days of the discharge from the hospital or the request for a visit from the participant (for Change Events). You MUST ensure the dates are correct and then select a corresponding reason.
Example:
Marital Status
- If the participant is listed as “Single” in Function Portal, double check if they have been married in the past (then change Function Portal if necessary)
- Partner/Significant Other are the same and include those the participant is romantically close to, without being legally married
- They may even refer to each other as spouses even if they aren’t actually married
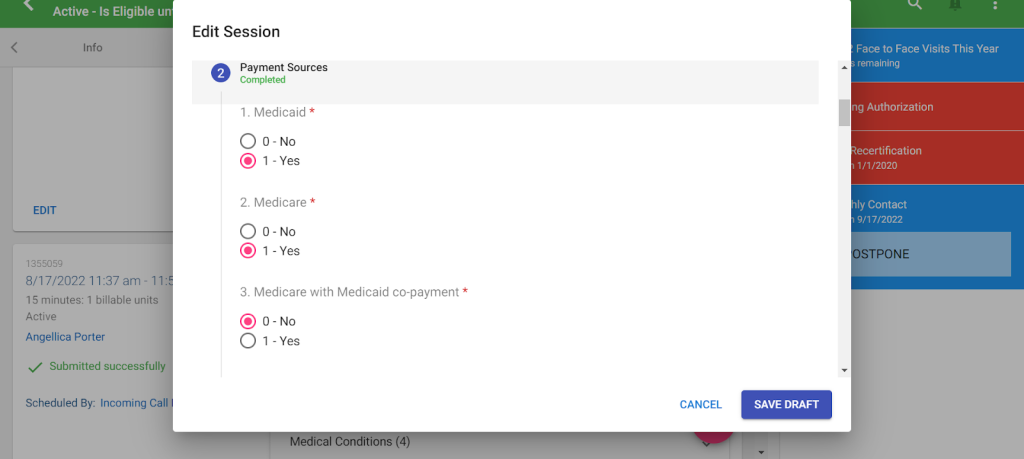
Payment Sources
Select Yes or No based on if the participant uses the following payment sources for Services. Information from this section MUST match the Info Tab in Function Portal.
Medicaid – All participants use Medicaid. Therefore the answer should be 1-Yes
Medicare – Answer will depend whether or not the participant has Medicare (check the Eligibilities tab in FP and verify with the participant during the visit
Medicare with Medicaid co-payment – Also known as the “Spend Down Program” Not common, answer is likely 0-No (verify with participant during the visit
- It is NOT about having a copay.
Example:
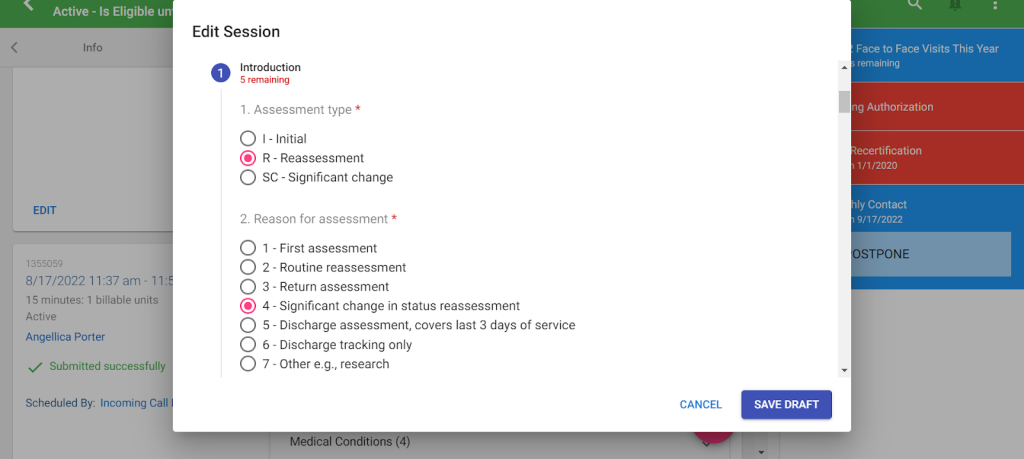
Reason for Assessment
Select the answer that applies to the type of visit you are completing, it must match
- New Participant Orientation (NPO) visits; answer is 1 – First Assessment
- Annual Visit; answer is 2 – Routine Assessment
- Change Event visit; answer is 3 – Return Assessment or 4 – Significant Change in Status Reassessment depending on why you are completing the visit.
- If you are doing the visit because you need to address a participant requesting a change in services (with no change in their health), or to follow up on a critical incident that did not actually change the participant’s health then select (3 – Return Assessment)
- If you are following up because there was a change in their health or caregiver, select (4 – Significant Change)
Example:
Person’s Expressed Goals of Care
- State the participant’s goal in having/receiving services and care in a full sentence.
- Then, state the goal again in just a couple of words below that
Example:

Intake and Initial History
More demographic and other general information about the participant.
Date Case Opened
This is the date the participant started with Amcord.
- This answer can be found in the participant’s Info tab on Function Portal, stated under Service Dates
- You must ensure the information on the Info Tab matches in all assessments
Primary Language
State the participant’s actual primary language. Not just the language they are speaking to you in, you need to verify this with the participant during the visit
Participant’s health and functioning
Cognition
This section is made up of questions regarding the participant’s cognitive ability to make decisions, maintain memory, and their awareness. If you indicate on the InterRAI that the participant has any issues with Cognition, then the PCSP must indicate the same information, as well as be consistent with the HRA/DSNP and the HEDIS. Higher scores mean more significantly impacted cognitive performance.
Memory Quiz – to test a participant’s short-term memory give them the following quiz. This is not a diagnostic tool. It just helps pave the way for better conversation on the topic if necessary.
- Ask the participant to remember 3 random objects
- Move on with more of the assessment, then in 5 min or so ask the participant if they remember the objects.
- If they forgot 2 or all 3 objects, then they may have a short-term memory problem.
- If they forgot only 1 object, then their short-term memory may be ok (or have more of a conversation with them about it)
- Ask the participant about the 3 objects again at the end of the assessment to test their Long-Term Memory.
Mood and Behavior
Discussion about the participant’s recent mental health and behavior.
Note: This section is specifically asking about indicators of the last 3 days.
Locomotion and Walking
Timed 4-meter walk
- Have the participant walk a straight, unobstructed path, across a room (about 13 feet) and time them. Your answer is how many seconds it takes for them to do so.
- If the participant needs to stop for any reason, stop and put answer 77 – Stopped before test complete
- If the participant refuses to do the walk, or you refuse to for any reason (including not being F2F) put 88 – Refused to do the test
- If the participant is not capable of walking in any way, put answer 99 – Not tested
Continence
Discussion about participant’s bladder and bowel continence control and use of any incontinence supplies.
If the participant requires or is requesting incontinence supplies, this section should indicate the need for supplies if the participant is requesting them at the time of the visit
Diagnosis and Problems
Documentation of the participant’s diagnoses. Pay close attention to the key/code and be sure to document any diagnoses the participant has.
- 0 – Not present – If the participant does not have the diagnosis
- 1 – Primary diagnosis – the primary reason why the participant requires care
- 2 – Diagnosis present, receiving active treatment – a diagnosis, besides the primary, for which the participant is currently being treated for
- 3 – Diagnosis present, monitored but no active treatment – a diagnosis, besides the primary, for which the participant is NOT receiving treatment for.
Other Disease Diagnosis – Listing any other diagnosis the participant has that was not listed in the previous questions
Example:

IADL’s (Instrumental Activities of Daily Living)
These are activities that are done daily or regularly to take care of the participant and their home. IADL’s require complex planning and thinking to complete. Discussion of how each activity is being performed currently should take place with the participant and their Person Centered Team, during the visit. Then select the option that most closely aligns.
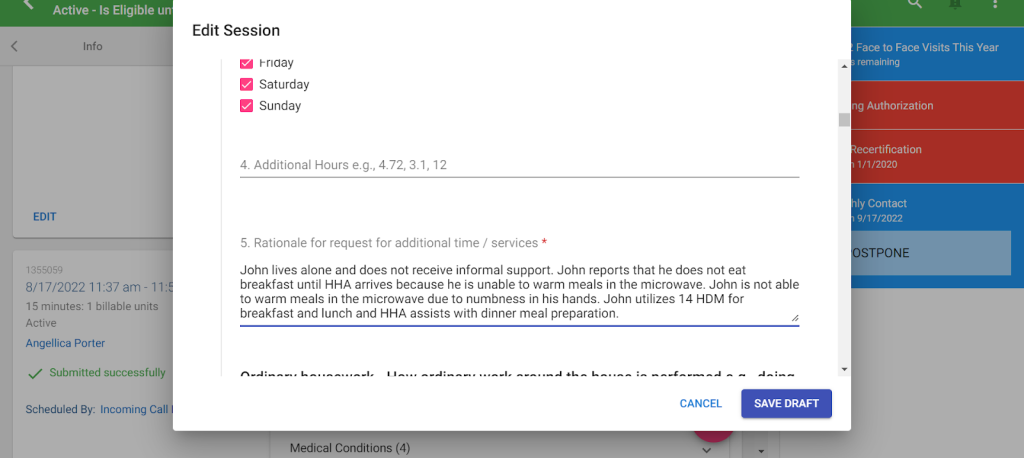
Example:

Discussion of what the participant’s capacity is to perform that same activity and what days they require assistance with this activity each week. It is okay if there is a difference between what is selected for “performance” and “capacity” (ie. A participant may have a daughter that currently makes all of the meals because she enjoys cooking for her mother, but the participant is capable of making small meals for herself at any time as well)
Please note: When selecting days of the week the participant requires assistance, this refers to ONLY days when formal assistance (ie. PAS hours) would be needed
Example:

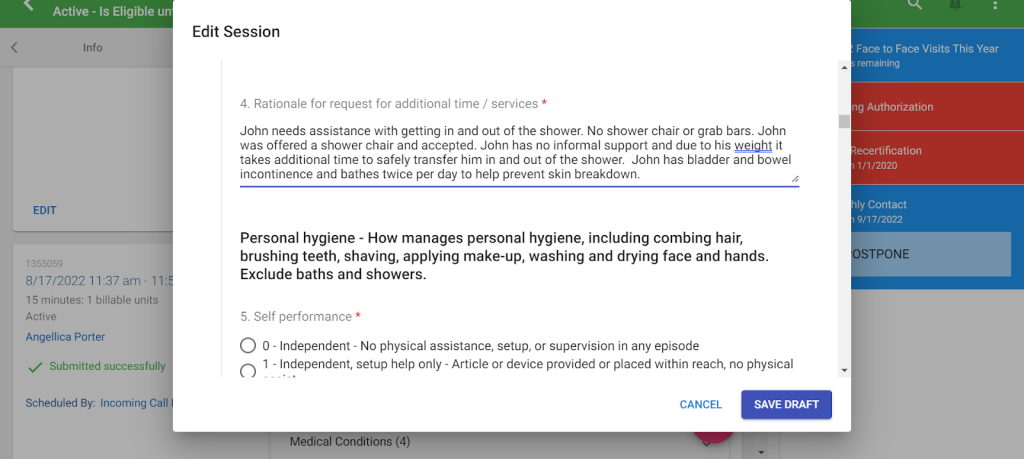
Discussion of the need for additional support to what is currently in place (either formally or informally) should take place. Additionally, rationale for all services must be included and this includes providing information on the following:
-whether the participant receives informal support or not for the specific task
-what services are currently in place and what other services were offered (ie. shower chair was offered and accepted OR shower chair was offered and declined)
-information about diagnosis or needs that are relevant to this activity
-clear statement on what the service that is put into place will be doing to assist (ie. HHA assists with meal preparation for dinner).
Example:
ADL’s
These are basic self-care activities that are done daily or regularly to take care of the participant and their home. Discussion of self performance of each task should take place with the participant and their Person Centered Team, during the visit. Then select the option that most closely aligns.
Please note: When selecting days of the week the participant requires assistance, this refers to ONLY days when formal assistance (ie. PAS hours) would be needed
Example:

The of days each week that the participant will need formal assistance should be discussed and corresponding days should be selected. Additional hours can be added, but only with justification.
Example:

Discussion of the need for additional support to what is currently in place (either formally or informally) should take place. Additionally, rationale for all services must be included and this includes providing information on the following:
-Whether the participant receives informal support or not for the specific task
-what services are currently in place and what other services were offered (ie. shower chair was offered and accepted OR shower chair was offered and declined)
-information about diagnosis or needs that are relevant to this activity
-clear statement on what the service that is put into place will be doing to assist (ie. HHA assists with meal preparation for dinner).
Example:
Additional Risk and Safety
Discussion of anything that does NOT fall under any of the ADL’s and IADL’s that would require additional hours, such as unsafe behavior (ie. turning the stove on and forgetting about it, wandering, etc) or high risk (ie. frequent falls and history of falls). There must be strong justification for what the presence of additional hours will resolve.
Example:


Narrative
This is a brief summary of the participant’s needs, their informal supports (must include “willing, able, available” language as well as name and relationship of informal), their current formal services, and what services they are asking for at this visit.
Example:

Discharge
If there was no hospital or NF stay then for “Last day of stay” you will type “12/31/2099”
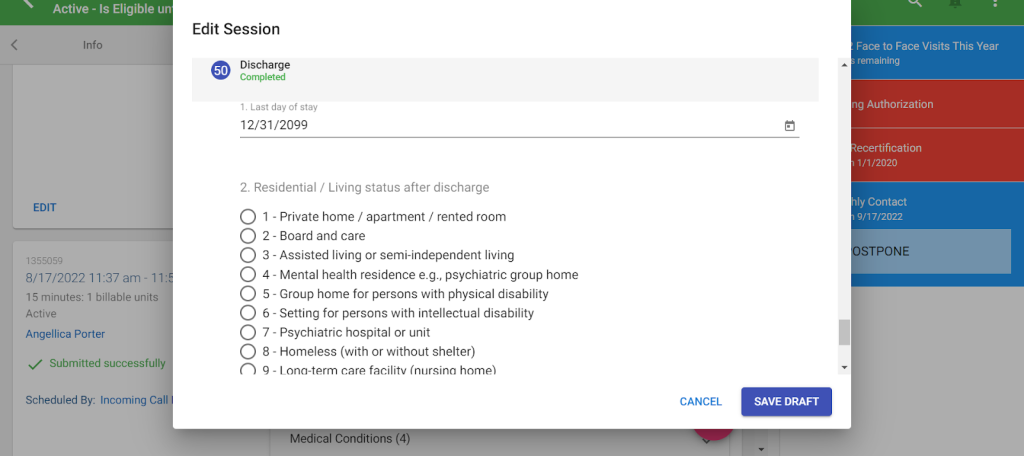
If there was no hospital or NF stay then for “residential/living status after discharge”, select “other”

Tips for IADL’s/ADL’s:
IADLs – Instrumental Activities of Daily Living
Self-care tasks that are necessary to live independently in the world. If these activities are not performed, it would result in a risk to a participant’s ability to live independently.
IADL Tasks
| Task | Details |
| Meal Preparation | -How meals are prepared-Includes: Planning/Deciding what food will be made for each meal, Preparing ingredients, Actually cooking and using appliances, setting up the dishes and utensils |
| Ordinary Housework | – How ordinary work around the house is performed – Includes: doing dishes, tidying up, dusting, vacuuming, making the bed, laundry, cleaning the bathroom. |
| Managing Finances | – How bills are paid, checkbook is balanced, household expenses are budgeted, credit card is monitored |
| Medication Management | – Includes: reminders to take medications, opening bottles, taking correct drug dosages, giving injections, and applying ointments |
| Phone Use | – How telephone calls are made or received Includes: assistance using assistive devices with phone use |
| Stairs | – How going up and down full flight of stairs is managed |
| Shopping | – How shopping is performed for food and household items – Includes: knowing what items are needed, choosing items, grabbing items and putting them in a cart, pushing a cart, paying money, bagging and carrying items. – EXCLUDE TRANSPORTATION |
| Transportation | – How participant travels by public transportation or drives themselves- Includes: navigating the public transit system, paying money for fares, getting in and out of the house and vehicles. |
IADL scoring
IADLs are scored separately based on Performance and Capacity
- Performance – the summation of actual performance of the task for the past 3 days.
- There is no speculation on the client’s or participant’s part. It is what was actually done.
- Capacity – the presumed capability of the participant to complete the task.
- This is gathered from conversation with the participant and caregivers as well as speculation of the participant. If you feel the participant is more or less capable of completing a task than was given in the performance, then the capacity score should reflect it.
Scores
| Score | Description | Example |
| 0 | Independent No help, setup, or supervision Meaning the participant does not need any assistance at all with the task. | Ex. The participant states they don’t need any assistance making or receiving calls |
| 1 | Setup Help Only The participant needs someone to set up all the necessary tools to complete the task, but then they can do the task without assistance. | Ex. The participant needs her daughter to get all bills and finances together, but once it is together the participant does the work themselves. |
| 2 | Supervision The participant needs someone to watch over them and make sure they do the task correctly, but still do all parts of the task themselves. | Ex. The participant needs their caregiver to remind the participant and make sure they take their medications, but they organize and take them by themselves. |
| 3 | Limited Assistance The participant can do the task themselves sometimes, but other times they need assistance. | Ex. The participant is able to make themselves a bowl of cereal or a sandwich, but needs assistance with more involved meals. |
| 4 | Extensive Assistance The participant needs assistance every time they complete the task, but are able to do more than half of said task on their own. | Ex. The participant goes shopping with a caregiver or informal support every time they need to go shopping, but they will push the cart, choose items, and pay for it themselves. The caregiver will grab items selected and carry heavy bags |
| 5 | Maximal Assistance The participant needs assistance every time they complete the tasks and they do less than 50% of the task themselves | Ex. The participant needs assistance for housework, they are able to use a duster on all reachable surfaces, but the caregiver or informal support does the high surfaces, vacuuming, mopping/sweeping, laundry, etc. |
| 6 | Total Dependence The participant has absolutely no involvement in the task. If it weren’t for the caregivers it would not be done. | Ex. The participant needs someone to take them upstairs, they cannot take any steps themselves and if no one is around they don’t go up or down stairs. |
| 8 | Activity did not occur In the past 3 days the task was not done at all. This is NOT used when scoring capacity (because capacity is based on some speculation.) | Ex. The participant has not left the house in the past 3 days and therefore did not need transportation anywhere. |
ADLs – Activities of Daily Living
Daily tasks that are necessary to remain healthy. If these are not performed it would result in immediate risk to the participant’s health or safety.
ADL – Tasks
| Task | Details |
| Bathing | – How a full bath/shower is taken – Includes: Transferring in and out of the tub/shower and how each part of the body is washed |
| Personal Hygiene | – How personal hygiene tasks are managed/completed. – Includes: washing face, brushing teeth, washing hands, putting on makeup, shaving, etc |
| Dressing Upper Body | – How dressing/undressing above the waist is managed. – Includes: underwear and outerwear, fastening buttons, zippers, prostheses, orthotics, etc. |
| Dressing Lower Body | – How dressing/undressing from the waist down is managed. – Includes: underwear and outerwear, fastening buttons, zippers, prostheses, orthotics, etc. |
| Walking | – How ambulation from one point to another is managed. – Includes: getting in and out of a bed, chair, or sofa, walking with or without assistive devices from one point to another while on the same floor. -Note: you should say “this activity did not occur” if the participant strictly uses a wheelchair or is bed bound |
| Locomotion | – How the use of durable medical equipment for ambulation (including wheelchairs) – Includes: if reminders or hands on help is provided to the participant to use assistive devices. – Note: the only time you should say “this activity did not occur” is if the participant does not use any assistive devices or if the participant is bed bound. |
| Transfer Toilet | – How they move on and off the toilet or commode. – Note: This is just for getting on and off of a toilet or commode. If the ptp is completely incontinent and does not use a toilet or commode, then this activity does not occur. |
| Toilet Use | – How using the toilet/commode/incontinence supplies is managed. – Includes: wiping themselves after going to the bathroom, either the toilet/commode or incontinence supplies, changing pads/diapers or other incontinence supplies, managing ostomy and/or catheters, readjusting clothes after going to the bathroom. |
| Bed Mobility | – How movement in bed is managed. – Includes: assistance moving from a lying position to sitting upright and vice versa, turning from side to side in the bed, changing positions in bed. |
| Eating | – How eating and drinking is managed- Includes: intake of food by other means such as tube feeding. – Note: It is NOT about set up of the meal, that is included in Meal Prep |
ADL scoring
ADLs are only scored on performance of the last 3 days
- If every single time the activity occurred was at the same level, then score the task at that level.
- Ex. If the participant says every time they take a bath/shower they just needed someone nearby to supervise, then you should give them the score for “Supervision”
- If any episode in the past 3 days was a 6, and others were less dependent, then score it at 5.
- Ex. If the participant says “Yesterday I was not able to move around in my bed at all, but today and most other days I can at least readjust myself” then you should give them a score of 5
- Otherwise, if the participant says their ability to complete tasks has fluctuated a lot in the last 3 days, focus on the 3 most DEPENDENT episodes. If the most dependent episode is a 1, then score it at 1. Otherwise score it 2-5 on the LEAST dependent episode
- Ex. In the past 3 days the participant has completed personal hygiene 7 times. Once they needed some weight bearing assistance (4), twice they needed limited assistance (3), every other time they needed set-up help (1).
- Therefore, focus on the weight bearing and limited assistance episodes. And you will score it on the least dependent of those episodes, limited assistance (3)
- Ex. In the past 3 days the participant has completed personal hygiene 7 times. Once they needed some weight bearing assistance (4), twice they needed limited assistance (3), every other time they needed set-up help (1).
ADLs Scores
| Score | Description | Example |
| 0 | Independent No physical assistance, setup, or supervision in any episode The participant does not need any setup help, supervision, or assistance at any point throughout the task. | Ex. The participant states they are able to feed themselves after all food is prepared and placed in front of them. |
| 1 | Independent, setup help only Article or device provided or placed within reach, no physical assistance or supervision in any episode. The participant needs someone to setup whatever is needed for the task, but then completes the task on their own. | Ex. The participant needs someone to place their hairbrush and toothbrush in reach and then is able to complete the task themselves. |
| 2 | SupervisionOversight/cuing The participant needs someone to watch over them and make sure they do the task correctly, but they still do all parts of the task themselves. | Ex. The participant is able to get a shower/bath themselves, but needs someone to watch over them to make sure they wash themselves fully and point out what they may have missed. |
| 3 | Limited Assistance Guided maneuvering of limbs, physical guidance without taking weight. The participant needs some physical assistance completing the task, but no weight bearing assistance. | Ex. The participant needs someone to guide their arms and legs into clothes when getting dressed, but does not need any weight bearing support at all. |
| 4 | Extensive Assistance Weight bearing support by 1 person where ptp still performs 50% or more of subtasks. The participant needs some weight bearing support by only one person when completing the task, but are still able to do 50% or more of the task themselves. | Ex. The participant is able to get up from the couch, needs to lean on the caregiver when walking into another room, but then is able to sit back down on their own. |
| 5 | Maximal Assistance The participant needs weight bearing support by 2 or more people OR they need weight bearing support for more than 50% of the task. | Ex. The participant needs someone to move her position in bed. She exerts some force, but heavily relies on caregivers to move her from lying to sitting up, vice versa, and rolling over in bed. |
| 6 | Total Dependence The participant has absolutely no involvement in the task. If it weren’t for the caregivers it would not be done. | Ex. The participant is not able to clean themselves up after incontinence episodes. They will sit in soiled garments until someone is able to change her. |
| 8 | Activity did not occur In the past 3 days the task was not done at all. | Ex. The participant does not use any assistive devices when ambulating. They walk on their own or with assistance from others. |
Rationale
The rationale is used to define the participant’s capabilities of completing each ADL and IADL as well as calculating how much paid caregiver assistance they need given their capabilities and support system.
This assessment is meant to be Person Centered. Therefore you should ALWAYS review this with the participant and/or responsible parties. NEVER assume information.
Every activity mentioned in the Rationales has to have a descriptive explanation of the care the participant requires, how it is conducted, how often it is needed, and who provides assistance. Gaps in care that may explain an increased request in hours should also be mentioned here.
Answer ALL considerations for each task in the chart below
| Details: | Considerations |
Meal Preparation All the steps of preparing all meals: – planning/choosing what to eat – preparing ingredients/supplies for cooking – Cooking and using appliances – Setting up food/dishes/utensils | HDM – Is the participant receiving HDM? – If so, state how many they receive along with how other meals are prepared throughout the day. – If not, were they offered? Were they accepted or denied? Meal details – How many meals need to be prepared? How long does each meal take to prepare? – Does the participant require a specific diet or modifications to their food? If so, why? Caregiver support – Does formal or informal support live with the participant and share the same meals with the participant? – If not, list the reasons why |
| Ordinary Housework Larger household tasks pertaining to safety and cleanliness: – Dusting/vacuuming – Mopping-Laundry – Cleaning kitchen/bathroom/living areas | Do NOT check off every day and do NOT add additional time. Home details – What type/size of residence does the participant live in. – Are laundry facilities located on site? – Does the participant live with others? – If the ptp lives with others, note that only the participant’s private areas are to be cleaned by the HHA (i.e. bedroom and bathroom). Otherwise, does the participant live with Informal support and are they able to assist? – If yes, what do they assist with? – If no, list the reasons why not. |
| Managing Finances All aspects of managing finances: – gathering financial document/resources -logging into and navigating online banking -balancing checkbooks/budgeting | – Do NOT check off more than 2 days and do NOT add any additional time – How does a caregiver assist? (i.e. HHA goes to the bank, HHA pays bills online, she reads them to the participant, HHA balances checkbook) |
| Medication Management -Reminding participants to take medications – Ensuring the participant does not choke | – PAS is only allowed to provide verbal reminders. They CANNOT administer medication and/or ensure participant is taking the correct doses. – Do NOT add any additional time. – How many medications does the participant take? – Does the ptp have Telecare medication dispensers? If not, was it offered and accepted? If not, why? |
| Phone Use How phone calls are made or received. | – Do NOT add additional time unless there is a legitimate reason such as having 6+ doctors and monthly appointments that need to be scheduled that the HHA assists with. – Do not add more than 0.50 hours. – Does the participant have any cognitive delays or difficulties with communicating? |
| Stairs How a full flight of stairs are managed -Going up and down 12-14 stairs at a time | Home Details – What type of home does the ptp reside in? – Where is their bedroom/bathroom? – Are there stairs inside and/or outside of the home? If so, how many? – If the ptp only has stairs outside of the home, ensure only the days the ptp leaves the home are selected. Ptp Health – Does the ptp have physical limitations caused by diagnoses? If so, describe them. – Does the ptp have any cognitive limitations, such as forgetting that they should not go up and down the stairs alone? If so, describe them. Has a Stair Glide been offered? – What was the ptp’s response to the offer? (i.e. Ptp refused stair glide or accepted it or does not own the home and landlord is not agreeable to stair glide). |
| Shopping How shopping for food and household items is managed: – knowing what items are needed – choosing items and carrying them/putting them in a cart – pushing a cart – paying for items – bagging and carrying items in/out of building/vehicles | -Do not select more than 2 days per week – How often do they shop? – Does the participant go out shopping with the caregiver or not? – Does the participant live with others? i.e Do they have informal support available to go shopping for them? – Are they receiving HDM and may not need as much groceries? Were they offered and if so list if accepted or declined – Do they have/use grocery delivery services available? |
Transportation How the participant manages using public or private transportation: – Navigating the public transportation system – Paying for fares – Getting in and out of the home and/or vehicles | Forms of transportation – Does the ptp receive a Septa Pass? If so, specify if the HHA goes with the ptp onto transportation and why (If HHA does not go with the ptp, do NOT add time for transportation) – This is NOT about time spent driving the ptp. HHA’s only assist with getting them in and out of the car. Therefore do not add time for length of travel. Reason for travel – Check off the appropriate amount of days with a relevant reason for travel (i.e. dialysis appointments 3x per week etc.) – Specify how often the ptp leaves the home and why. |
| Bathing How a full bath/shower is completed: – getting in and out of the tub/shower – Setting up assistive devices for bathing/showering – Washing and drying each part of the body (except hair and back) – Bed bathing the participant along with set up to do so | Review Board recommends bathing only one time a day. (due to increased risk of skin breakdown) – If the ptp is incontinent, make sure it is defined in the rationale and in Section H. Explain why multiple baths might be needed for that participant throughout the day. Home Mods/DME – What DME/Home mods does the ptp have already? List the items – If none, were they offered? (i.e. Home Mods, shower chairs, grab bars). Were they accepted or denied? – If accepted, does the ptp own the home? – If denied, explain why. Caregiver Support – How does the caregiver assist the ptp? – How much time is spent to complete the bath/shower? |
| Personal Hygiene Completing all personal hygiene tasks: – Combing/brushing hair – Shaving- brushing teeth – applying make-up – washing/drying face and hands | – Do NOT duplicate justification from bathing. – Does the HHA provide set up or hands-on-help? – What can the ptp do independently? -What does the informal assist with? |
| Dressing Upper Body How they dress/undress the upper body: – choosing appropriate clothing – putting on bra -pulling clothes over their head -putting arms through the sleeves -Fastening buttons/zippers | – Why does the ptp need assistance? – What can the participant do independently and what does the HHA do to assist? – Is informal support available to assist? |
| Dressing Lower Body How they dress/undress the lower body: – choosing appropriate clothing – putting on underwear – stepping into clothes and pulling them up to the waist (if applicable) – Fastening buttons/zippers | – Why does the ptp need assistance? – What can the participant do independently and what does the HHA do to assist? – Does the participant have buttons/zippers – Is informal support available to assist? |
| Walking How the participant walks from point A to B – Completing additional physical/occupational therapy exercises -Getting on and off chairs, sofas, bed, etc. | – Does the participant require supervision or physical assistance while walking? If so, why? – Does the participant have any assistive devices? (ie. walker, cane, wheelchair) – If so, describe them – If not, were they offered? – How many trips to the bathroom per day does the participant require assistance? |
| Locomotion How the participant receives assistance with assistive devices when walking or with a wheelchair: -Retrieving/setting up assistive devices -Reminders about using assistive devices -Being pushed in a wheelchair | – Do NOT duplicate information from the walking section – What assistive devices does the ptp use? – What assistance is provided for use of canes/walkers/wheelchairs? (i.e. reminders to use cane, needs walker brought to them, needs to be pushed once in their wheelchair) – What is the participant able to do on their own? -Should the next level of device be offered (ie. if ptp needs maximum help to move with the walker and is still struggling, have we offered a wheelchair or recommended they talk to PCP about one?) |
Transfer Toilet Assistance getting on and off of a toilet or commode: -GOING TO AND FROM THE BATHROOM is NOT included | – Do NOT include time walking to the bathroom – Who assists the participant? – How many times a day does the ptp go to the bathroom on average? – Does the participant have any Home mods, DMEs, or SMEs? (i.e grab bars, raised toilet seat, commodes, urinals)- If yes, state them- If no, were Home Mods/DME/SME offered? Did the participant accept or deny? – Does the ptp have any incontinence diagnoses or take any medications that affect balance during transfers? |
| Toilet Use -Assistance using the toilet and/or commode/urinal or management of incontinence supplies -wiping/cleaning themselves -changing pads/incontinence supplies -managing ostomy/catheters -re-adjusting clothes | – Do NOT include time walking to the bathroom – Does the participant use the toilet, incontinence supplies, or both? Describe why the participant uses any devices – How many times a day does the ptp go to the bathroom on average? -What assistive devices have we offered (ie. commode, urinal, raised toilet seat, incontinence supplies) and were they accepted or declined |
| Bed Mobility -Moving/changing positions in bed – moving to and from lying down to sitting up – moving from side to side in the bed/rolling over – changing position in the bed | – What assistance is provided? (i.e. HHA provides assistance by handing cane and helping to transfer in and out of bed). – How many times per day OR how often does the ptp require assistance (i.e. helping twice per day or repositioning every 2 hours to prevent bed sores) – Was DME offered? (i.e. Hoyer Lift?) |
| Eating -How the participant eats/drinks? – includes tube feeding and other means of eatingbeing fed and supervision to prevent choking | – Do NOT include time for setting up food/dishes and/or modifying food. That is for Meal Prep – Does the participant need assistance being fed or given reminders to eat due to diagnoses. – Does the participant eat orally or through tube feeding? |
| Additional Risk/Safety Care that the ptp requires outside of the standard ADLs and IADLs (I.e. Wandering, unsafe behavior, memory issues, frequent falls) If you are not sure about Risk/Safety, discuss the situation with your Supervisors | – Specific IADL/ADL assistance should NOT be a part of this justification. (I.e. if additional support is needed for walking through the house, put that in “Walking”) – Some examples of acceptable Diagnosis where Risk and Safety could be justified are Alzheimer’s, Dementia, Multiple Sclerosis, Cerebral Palsy, etc.***Just because the ptp has the diagnoses does NOT mean they automatically get risk and safety. Only if there is a need for it.*** – Do NOT list Behavioral Health diagnoses as needing supervision. If you feel the ptp needs more support due to BH diagnoses, talk to your Supervisors and make a referral. – A High risk score may or may not be justification for risk/safety hours, but additional information on why there is a high risk score will be needed. (I.e. Risk score of 35, because participant is wandering each night and has had 4 falls in the last week and participant has no informal supports) – If you are not able to properly explain how adding risk/safety time would decrease the ptp’s risk and/or increase their safety, then it is likely not appropriate to put hours into this section. |
| Rationale for Narrative Summary of care and amount of hours needed/received/being requested | Visit time– State the time spent with the participant/care team (I.e. “Visit start time: 10a – End Time time: 11:35a” Authorization vs. Request– State the amount of hours the participant is currently authorized for vs. the amount they are requesting to receive vs. the amount the SPG Tool reveals. Informal Support– Any Informal supports stated must be detailed here, as well as in the PCSP – MUST state that informal supports are willing, able, and available to assist the ptp and the ptp agrees (I.e. Ptp’s son/John Smith is willing, able, and available, but the ptp does not want them to assist with toileting or dressing tasks due to the ptp wanting privacy OR Ptp’s daughter/Betty Smith verbally confirmed she is willing, able, and available and will assist with bathing, dressing, shopping, managing finances, and transportation to medical appointments each week). |



Sorry, the comment form is closed at this time.