24 Apr Person Centered Service Plan (PCSP)
The PCSP is the document where all of the participants current and requested services are listed, along with goals that the participant has chosen to work towards. A PCSP needs to be done, with several other documents, at every New Participant Orientation (NPO), Annual, or Change/Trigger Event. Once a visit is scheduled in Function Portal, the SC clicks the “Document” button to begin working in the assessments that are listed in the Alerts on the right hand side of the screen.

The following all need to be included in the PCSP session in Function Portal:
- All currently authorized services
- Use the authorization spreadsheet for reference
- Use the guide below to document any requested changes to current services (Increases, Decreases and Termination)
- Any other services the participant receives
- i.e. Transportation services, DME/SME, and any other Medicare and other payor covered services
- Behavioral/Mental Health Services
- Employment Services
- Any new Medicaid services being requested
- Informal Support, even if the participant has no informal support, this needs to be documented
PA Health and Wellness will make the final determination for services. Participants will be notified via a determination letter from PHW
Service Plan Breakdown

- Type of Service – the needed service
- The first Service will always default to Service Coordination
- There must always be at least 2 services for any active participant
- Select the appropriate service type
- Service Amount/Frequency – the amount of service authorized based on the frequency
- Frequency and amount is specific to each service and should come from the Authorization sheets sent each day
- Service Details – A brief description of what the service provides. Be specific to the participant’s needs.
- Service Provider and Delivery – The provider chosen by the participant (if applicable) and delivery method
- If the provider is Tempus (PDO), select Participant Directed – Employer Authority for Delivery Type
- If the provider is anything other than Tempus, select Agency Option for Delivery Type
Entries for common services
Personal Assistance Services (PAS)
AGENCY OPTION
Service Type: Personal Assistance Services
Service Details: State the specific ADL’s and IADL’s the participant requires
Amount: Amount of hours CURRENTLY authorized (regardless of request/SPG tool) per week
Frequency: Weekly
Delivery: Agency Option
Provider: Agency Name, phone number, address, and agency NPI #
PARTICIPANT DIRECTED OPTION (PDO)
Service Type: Personal Assistance Services
Service Details: State whether it is Regular Time or Overtime and state the specific ADLs and IADLs that this participant requires caregiver assistance with, this should be different for every participant.
Amount: Amount of hours CURRENTLY authorized (regardless of request/SPG tool) per week
Frequency: Weekly
Delivery: Participant Directed – Employer Authority
Provider: Tempus (PDO) 844-983-6787
Personal Emergency Response System (PERS)
EXISTING SERVICE
Service Type: Personal Emergency Response System
Service Details: Monthly Maintenance + description
Amount: 1
Frequency: Monthly
Delivery: Agency Option
Provider: Agency Name, phone number, address, and NPI
NEW SERVICE
When putting in a new PERS unit request you will need to have 2 separate services.
1. One for Monthly Maintenance Request (see above)
2. Additional One Time Installation Request
Service Type: Personal Emergency Response System
Service Details: One Time Installation + description
Amount: 1
Frequency: One Time
Delivery: Agency Option
Provider: Agency name, phone number, address, and NPI
Home Delivered Meals
Service Type: Home Delivered Meals
Service Details: Description + diet requirements (ie. diabetic appropriate, etc), preferences, or restrictions (ie. allergies, cultural needs,etc)
Amount: # of meals received per week (Max 14)
Frequency: Weekly
Delivery: Agency Option
Provider: Agency name, phone number, address, and NPI
Transportation Services
NON-MEDICAL TRANSPORTATION (MTM RIDES)
Service Type: Non-Medical Transportation
Service Details: Service description + average amount of round trips needed per week
Amount: Average amount of trips needed per month (average amount of round trips x 8)
Frequency: Monthly
Delivery: Agency Option
Provider: Medical Transportation Management (MTM) | 888-561-8747
NON-MEDICAL TRANSPORTATION (SEPTA KEYCARD)
Service Type: Non-Medical Transportation
Service Details: Service Description + Zone ptp requires
Amount: 1
Frequency: Monthly
Delivery: Agency Option
Provider: Medical Transportation Management (MTM) | 888-561-8747
NON-MEDICAL TRANSPORTATION (CCT PASS)
Service Type: Non-Medical Transportation
Service Details: Service Description + Zone 2 + Utilizes CCT
Amount: 1
Frequency: Monthly
Delivery: Agency Option
Provider: Medical Transportation Management (MTM) | 888-561-8747
MEDICAL TRANSPORTATION (MATP)
Service Type: Other
Service Details: Service description
Amount: 1
Frequency: Monthly
Delivery: Agency Option
Provider: Medical Assistance Transportation Provider (MATP) | 877-835-7412
Adult Day Care/Center
Service Type: Adult Daily Living
Service Details: Service description
Amount: number of days attending per week
Frequency: Weekly
Delivery: Agency Option
Provider: Agency name, phone number, address, and NPI
Home Mods
Each requested Home adaptation requires its own service entry. Home mods should not be added to the Service Plan until after all Proof of Home Ownership documents are received.
Service Type: Home Adaptations
Service Details: “Home adaptations evaluation is required …” then state the barrier the home mod is meant to overcome (ex. participant cannot go up and down steps to the second floor where the bedrooms and bathrooms are)
Amount: 1
Frequency: One Time
Delivery: Agency Option
Provider: TBD
Durable Medical Equipment (DME)
Each DME and SME requires their own service entry. DMEs and SMEs should NOT be added to the PCSP until AFTER they are being received.
Service Type: Specialized Medical Equipment and Supplies
Service Details: description of item including size if applicable
Amount: 1
Frequency: One Time
Delivery: Agency Option
Provider: Provider name, phone number, address, and NPI
Specialized Medical Equipment (SME)
Each DME and SME requires their own service entry. DMEs and SMEs should NOT be added to the PCSP until AFTER they are already being received.
Service Type: Specialized Medical Equipment and Supplies
Service Details: description of item including size if applicable and average amount being used per day.
Amount: average amount needed per day
Frequency: Daily
Delivery: Agency Option
Provider: Name and phone number of provider
Exceptional Durable Medical Equipment
Any item that is custom to the participant (i.e. it cannot be used straight out of the box) and the cost is equal to or greater than $5,000 is considered Exceptional DME (EDME) and is required to be added to the PCSP and an SRT must be completed
Service Type: Exceptional DME
Amount: 1
Frequency: One Time
Delivery: Agency Option
Provider: Provider name, phone number, address and NPI of chosen provider or TBD
Informal Support
Service Type: Other
Service Details: ADLs and IADLs that informal support assists with AND description of how/when informal support confirmed their role. Ex. “During assessment, Example verbally stated they are willing, able, and available to provide informal support”
Amount: Amount of hours Informal support agreed on per week
Frequency: Weekly
Delivery: Agency Option
Provider: Full name and phone number of Informal supporter(s)
Service Format based on scenarios
Services Staying the same as prior Service Plan
If a SC has completed an assessment with a participant, in which services and providers are all staying the same as the last assessment, then the Service Plan in the PCSP should reflect the following:
- Amount: The amount currently authorized
- If PHW makes a change to the PAS hours that will be approved moving forward (e.g. increase or decrease), at the next visit with the participant the SC will update the PCSP Service plan to reflect what is currently approved.
Increase/Decrease Procedure
FOR PAS
If SC has completed an assessment with a participant and the hours for PAS indicated by the new assessment are either an increase or a decrease from what the participant has currently, then the Service Plan in the PCSP should reflect the following:
- Amount: The amount currently authorized (this will not match the SPG Tool)
- If PHW makes a change to the hours that will be approved moving forward (e.g. increase or decrease), at the next visit with the participant the SC will update the PCSP Service plan to reflect what is currently approved.
FOR NON-PAS
If SC has completed an assessment with a participant and an increase or decrease in a Non-PAS service are being requested, then the Service Plan section of the PCSP in Function Portal should reflect the following:
- Amount: Increase/decrease amount being requested (ie. 14 meals per week) and specify the end date in the details if appropriate
New service request
FOR PAS
If SC completes an assessment with the participant and a request is made for PAS and the participant does not currently have PAS hours, then the Service plan in the PCSP should reflect the following:
- Amount: will be “0”
- PA Health and Wellness will make the final determination of hours.
- At next visit with the participant SC will update assessment to reflect currently authorized PAS hours
FOR PERS
For a PERS installation, you need to also make two separate services.
- First service: PERS installation
- Amount: 1
- Frequency: One time
- Second Service: PERS Monthly Monitoring
- Amount: 1
- Frequency: Monthly
FOR EVERY OTHER SERVICE
If SC completes an assessment with the participant and a request is made for a Non-PAS service (e.g. HDM’s, transportation, etc) and the participant does not currently have that service, then the Service plan in the PCSP should reflect the following:
- Amount: amount that is being requested
Ending a Current Service
DO NOT just leave the service off of the service plan
If SC has completed an assessment with a participant and it has resulted in a request to end a service that is already in place.
- Amount: amount of service approved will be “0” and specify the end date in the details of that service
Change in Provider
This will result in two separate entries on the PCSP for the same type of service
If SC has completed an assessment with a participant and a change in any type of provider is being requested, then the Service Plan in the PCSP should reflect the following:
- 1st Entry
- Amount: Current amount of service approved
- Specify the end date for the 1st Provider in the Service Details
- 2nd Entry
- Amount: Current amount of service approved
- Specify the start date for the 2nd Provider in the Service Details
Needs, Goals, and Outcomes Overview
Overview
The Needs, Outcomes, and Goals are made based on the participant’s services and their personal goals. There must be a Need, Outcome, and Goal for each service (except Service Coordination*) until you run out of available Needs/Outcomes/Goals in the “Person Centered Care Plan and Outcomes” section of the PCSP in Function Portal. If you have a N/G/O for each service and there is additional room, then the participants personal goals should be listed.
Needs
Details why the participant Needs the service or what they need help with specifically requiring the service. Always ask the participant “Why do you need this service?” or “what does this service help you with?”
- When documenting needs in the PCSP in Function portal, select the most appropriate option that matches the participants need

If there is no need that matches, select “Participant needs something else” and then specify the need in the following format.
Examples of Needs for common services:
PAS
Why does the participant need a caregiver/what is the caregiver going to help them with?
- Ms. Amcord needs to eat diabetic appropriate meals to prevent hospitalizations for high glucose levels
- Ms. Amcord needs to take her medications as prescribed
- Ms. Amcord needs to improve mobility
- Ms. Amcord needs to improve personal hygiene
- Ms. Amcord needs to decrease hospitalizations related to falls that take place while completing bathing, dressing, and ambulation
PERS
Why does the participant need a PERS unit/what will the device do for them?
- Ms. Amcord needs to be able to access EMS and is unable to dial a phone
- Ms. Amcord needs to be able to attain assistance from EMS should a fall/injury take place
HDM
Why does the participant need home delivered meals/what will the meals provide them?
- Ms. Amcord needs to better manage her health through diet and nutrition
- Ms. Amcord needs to better manage her diet and food portion intake
- Ms. Amcord needs to have access to 2 meals per day to maintain her physical well being
- Ms. Amcord needs to prevent hospitalizations due to high glucose levels
ADC
Why does the participant need to attend ADC?
- Ms. Amcord needs to improve her socialization skills
- Ms. Amcord needs to have constant supervision and assistance with bathing, dressing, and toileting throughout each day
- Ms. Amcord needs to improve her depression and anxiety
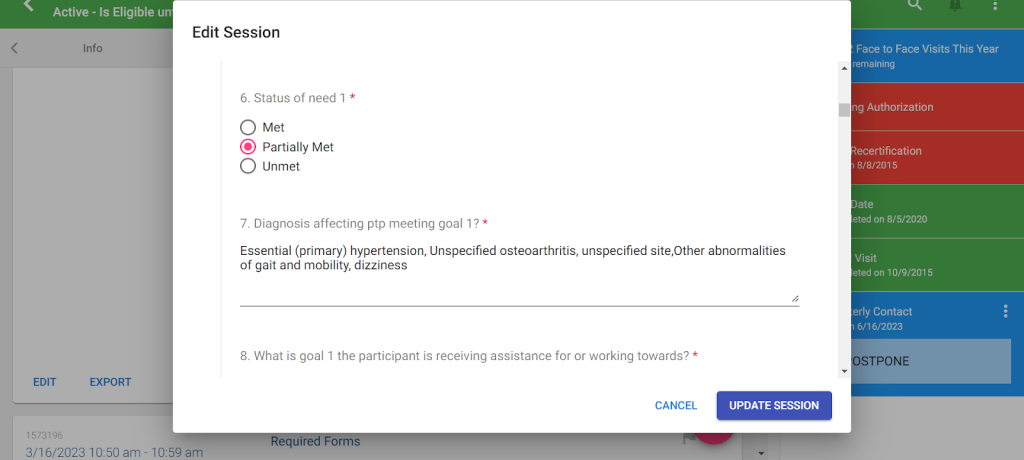
Status of Need
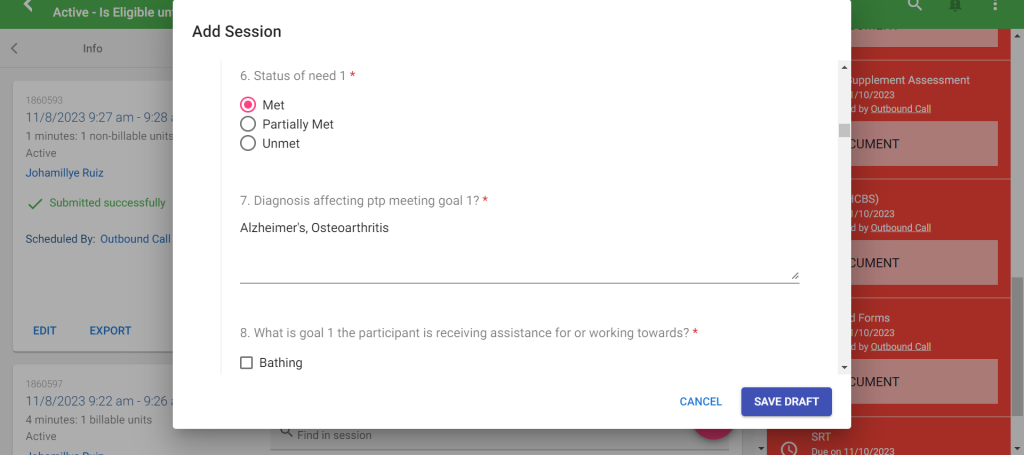
Met: This indicates that the Need is already being addressed fully, through either informal, formal, or a combination of both types of assistance.
- If there is already a service in place (ie. PAS) to meet the need and there is no area of the need being unmet, then you would select “met”
- Ie. Participant has PAS provide verbal reminders during shifts to take medications, participant is taking medications 100% of the time.
Partially Met: This indicates that the Need is only partially met at the time of assistance
- If there is already a service in place (ie. PAS) to meet the need, but it is not fully met, then you would select “partially met”
- ie. Participant has PAS provide verbal reminders during shifts to take medications, but the participant is forgetting to take medications during times when PAS is not present.
- Service Coordinator should ensure a service is put into place to meet the need moving forward
Unmet: This indicates that the Need is unaddressed by either formal or informal assistance at this time.
If there is no service in place yet and the need is not met OR there is a service in place but it is not meeting the need, then you would select “unmet”.
- ie. Participant has no services yet that assist with medication reminders and is currently forgetting to take medications each day, the participant does not have family or friends to assist.
- Ie. Participant previously wanted PAS to remind them to take medications daily, but the participant wants the PAS schedule to be at times when the participant would not be taking medications. Participant is currently forgetting to take medications and does not want to move the PAS schedule.
Service Coordinator should ensure a service is put into place to meet the need moving forward
Outcomes
Details the Outcome on the participant’s life/health/well-being if the Need is satisfied.
Always ask the participant, “What are you hoping to achieve by satisfying the previously stated need?“
- When documenting Outcomes in the PCSP in Function portal, select the most appropriate option that matches the participants Need selection
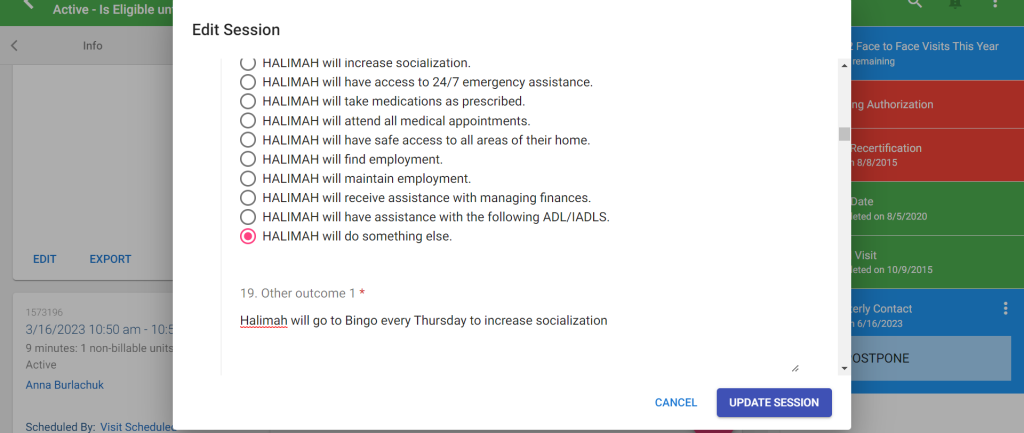
If there is no Outcome that matches, select “will do something else” and then specify the desired outcome
Goals
Details the participant’s Goal in having, receiving, or utilizing the service to satisfy the Need and obtain the desired Outcome. Goals are automatically built in SMART format, after the necessary goal related questions are answered.
1. List what diagnosis is causing the participant to experience the Need
2. Select from the list, what the goal is working towards
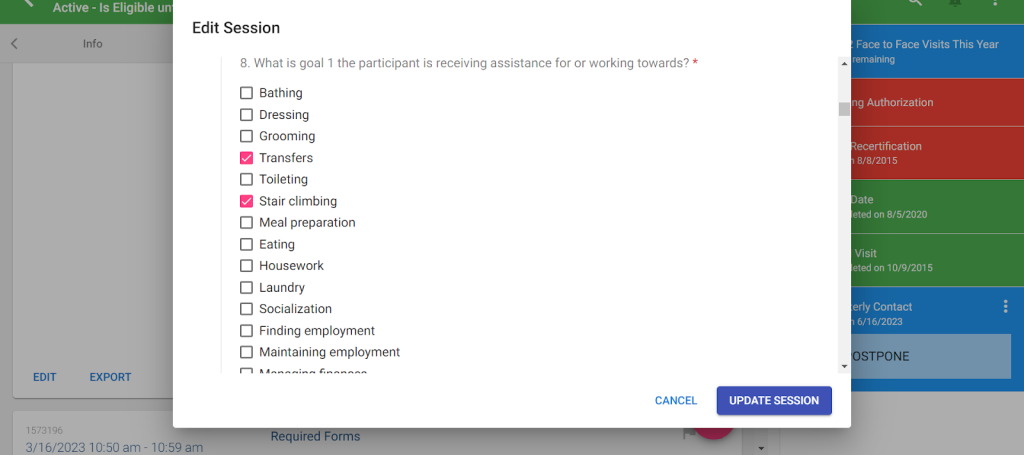
If no option from the list in Function Portal matches what the participant is looking for, select “other” and then write in one or two words that sum up what the participant is working towards.

3. Select from the list, who will assist the participant with meeting the goal
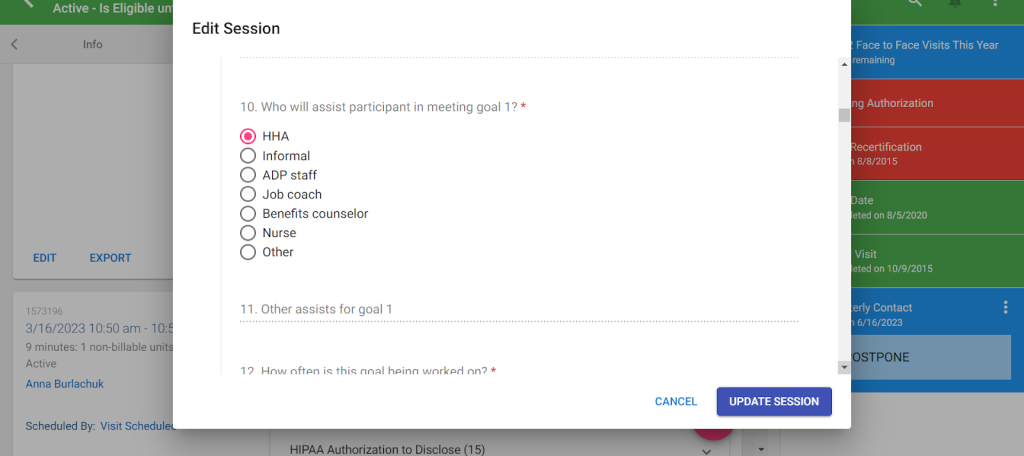
If no option from the list in Function Portal matches who will be helping the participant, select “other” and then write in the position of the person assisting (ie. Physical Therapist, NF staff, etc).
4. Select from list, how often the goal is being worked on

If no option from the list in Function Portal matches how often the participant will be working on the goal, select “other” and then write in the frequency that is appropriate.
Barriers
Something that prevents the participant from achieving their goals. If a participant has no informal supports this needs to be documented in the barriers. Any cognitive issues must be addressed in the barriers. There are no times where a participant does not have at least one barrier to any given goal.
- Select from the options in Function Portal, all of the barriers that the participant has related to the goal

If no option from the list in Function Portal matches how often the participant will be working on the goal, select “has another barrier” and then write in the frequency that is appropriate.
Intervention
What can/will be done to overcome the barrier and proceed with achieving the goal. If a participant has informal support they need to be listed in the interventions with the specifics of what they will be assisting with.
- Select from the list in Function Portal the appropriate response for Interventions that will be used

If no option from the list in Function Portal matches the Interventions that will be used to assist the participant, select “will receive something else” and then write in the intervention that is appropriate.
Cognitive Issues Guide
Cognitive Issues
We are responsible for ensuring that when we document that a participant has a cognitive issue that we are also documenting how those cognitive issues will be addressed, inside of the HEDIS note. There needs to be consistency between all of the different assessments.
This applies to both Nursing Facility participants and Home and Community Based Services participants.
NF participants- if there is a cognitive issue indicated in any part of the HEDIS then the PCSP
must address the cognitive issue and plan to address it is captured in the HEDIS.
HCBS participants- if there is a cognitive issue indicated in any part of the HEDIS or InterRAI then
the PCSP must address the cognitive issue and the plan to address it is captured in the HEDIS.
There are a few different ways that we might be able to show that we addressed the issue:
- Medication Management- ptp may use Telecare, blister packets, or someone to assist with verbal
reminders to take medications.
- Financial Management- ptp may have someone else paying the bills due to confusion.
- Phone use- ptp may receive assistance with setting up medical appointments due to forgetfulness.
- Other- the ptp may have a unique situation where their cognitive issue affects one of the other ADL/IADL’s.
Below you will find some examples of how to handle the documentation for participants with a cognitive issue.
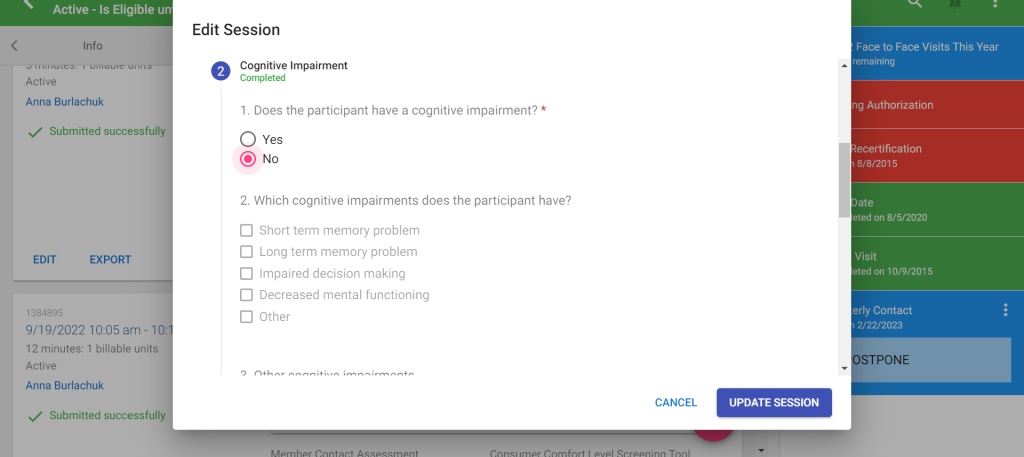
Example if ptp who does NOT have cognitive issues:
- The “cognitive issue” box is not selected in the PCSP.
- In “Barriers to any of the above” it clearly states there are no cognitive issues, in the PCSP.
- No portion of the InterRAI and/or HEDIS related to cognition or memory issues is selected.
You must ensure that ALL steps are completed for a ptp with no cognitive issues.
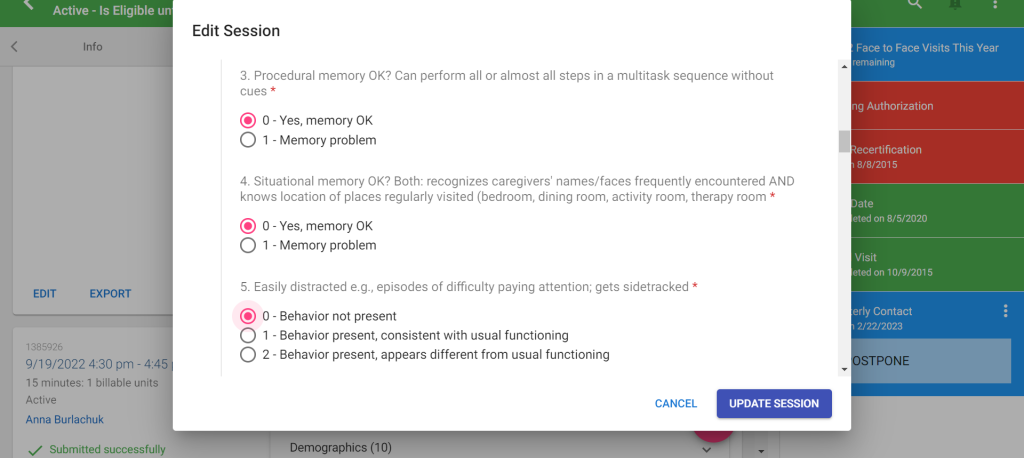
Example InterRAI for a participant with no cognitive issues:


Example PCSP in Function Portal for a participant with no cognitive issues: (you must state there is no cognitive issue).

Example of HEDIS for participant with no cognitive issues:
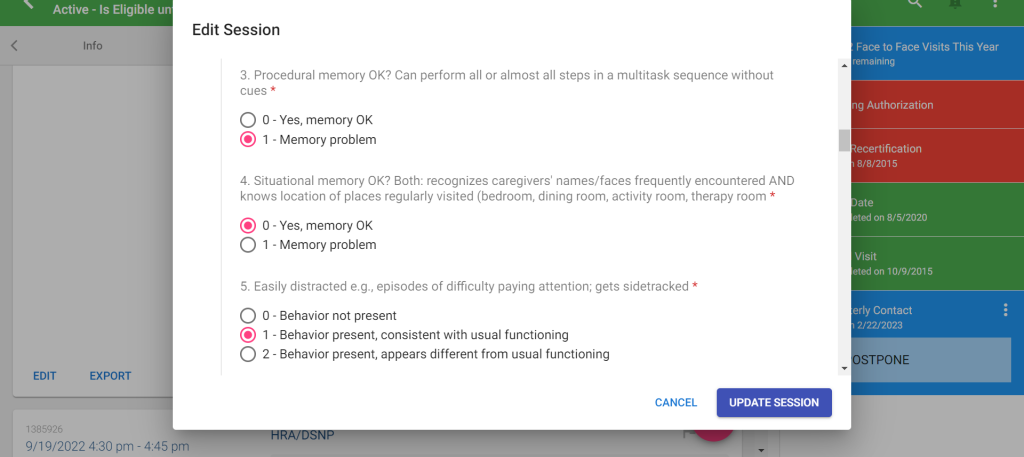
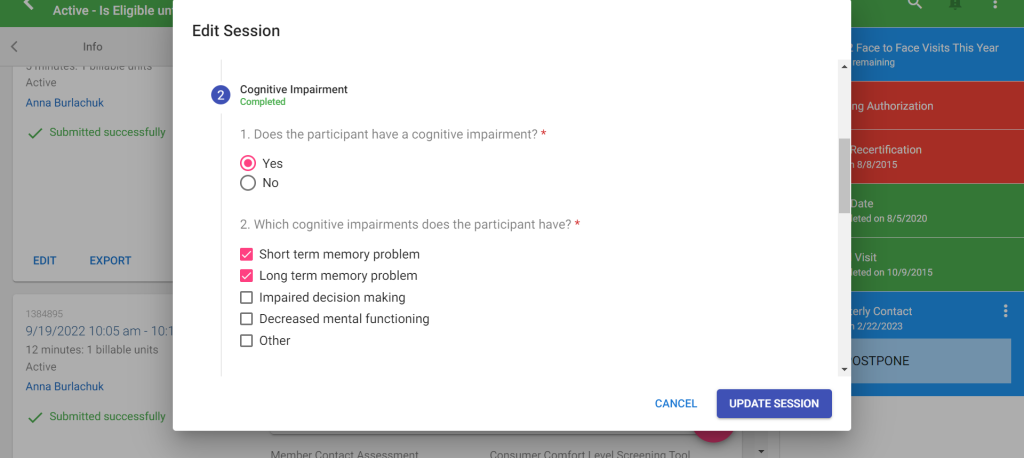
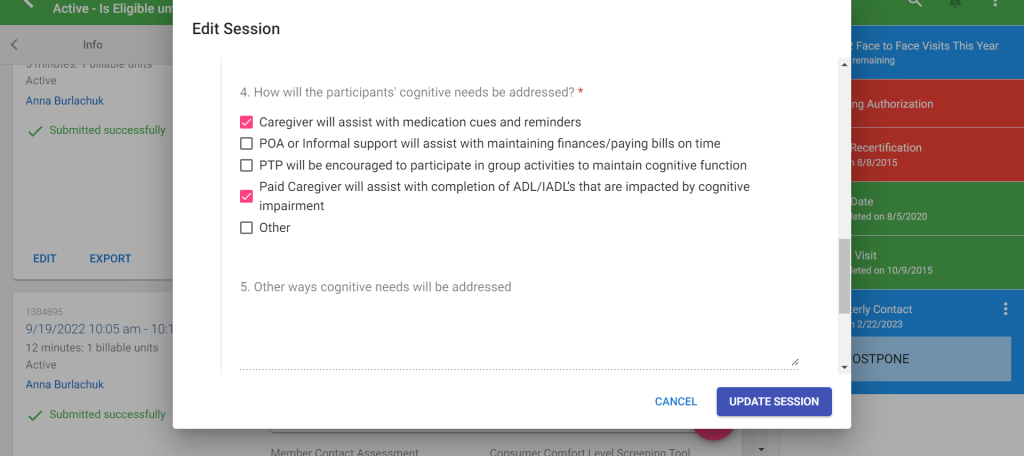
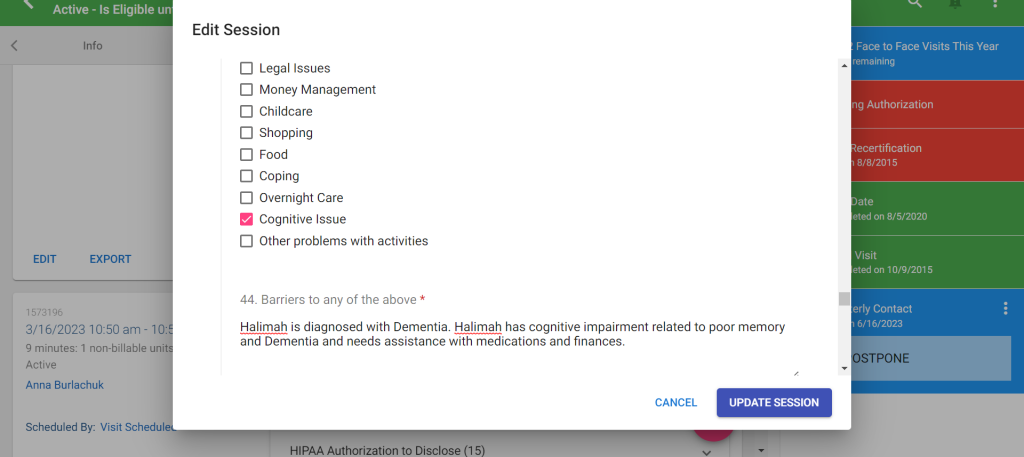
Example if ptp who has cognitive issues:
- “Cognitive issues” box is checked off in the PCSP in Function Portal
- In “Barriers to any of the above” the cognitive issue is stated along with what ADL/IADL it affects and how it is addressed, in the PCSP in Function Portal.
- InterRAI and/or HEDIS have corresponding information in regards to cognitive issues.
- Even if a participant reports that they have a cognitive impairment that does not impact their daily functioning (ie. only cognition issues in new situations), this MUST be treated as a cognitive issue.
Example of InterRAI for participant with cognitive issues:

Example of HEDIS for participant with cognitive issues:
Example of PCSP for participant with cognitive issues:
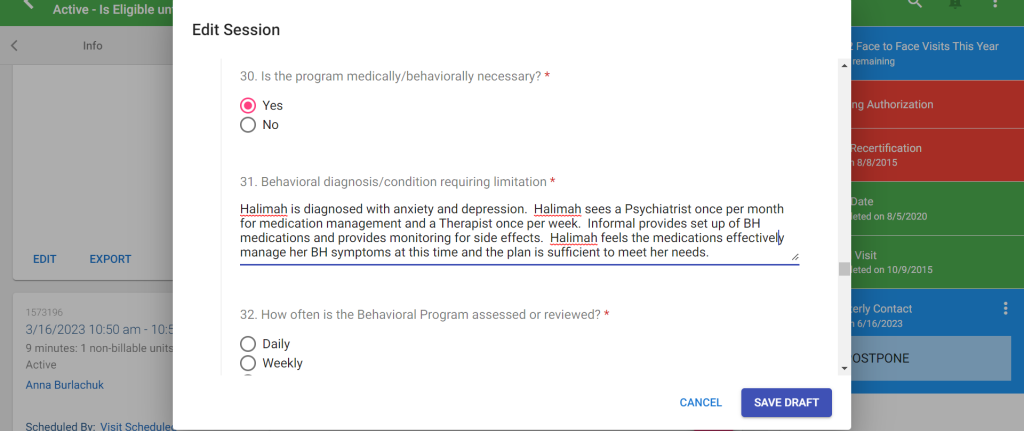
Mental Health Plan
- We need to ensure that for all participants that have a Mental health diagnosis that we are capturing the plan for how their mental health is being managed.
- Examples of Mental Health Diagnosis
- Depression
- Anxiety
- Schizophrenia
- Borderline personality Disorder
- Post Traumatic Stress Disorder (PTSD)
- Bipolar Disorder
- If you are unsure if a current diagnosis that the participant has falls into the category of Mental Health, then please follow up with your supervisor for guidance.
- Examples of Mental Health Diagnosis
- Mental Health information is captured in the PCSP
- You will need to gather information from the participant/POA during the visit to document a plan.
- Examples of questions to ask at the visit
- Do you currently take any medications to treat the diagnosis?
- Who prescribes the medication? (ie. Psychiatrist or PCP)
- How often do you see the prescribing physician?
- Does anyone assist you with taking or remember to take these medications?
- Does anyone help monitor the effectiveness of your medication?
- Do you see a Therapist? If so, how often do you see them?
- Examples of questions to ask at the visit
- Examples of ways that Mental health plan can be documented appropriately
- Mrs. Smith is diagnosed with anxiety and depression. Mrs. Smith sees her PCP/Dr. Doe every month to review the effectiveness of her mental health medications. Mrs. Smith has assistance from her HHA to remember to take her MH medications each day. Mrs. Smith reports that her current medications are managing her diagnosis effectively at this time.
- Mr. Smith is diagnosed with schizophrenia and sees his Psychiatrist/Dr.Wright once every other month for medication review. Mr. Smith’s daughter/Betty Smith provides supervision to ensure Mr. Smith is not exhibiting any unsafe behaviors and also monitors for medication effectiveness. A medication dispenser is used each day to ensure Mr. Smith takes his MH medications as prescribed.
- Mrs. Smith is diagnosed with depression and anxiety. Mrs. Smith reported that she is not taking medication for these diagnoses and is not interested in a Behavioral health referral at this time. Mrs. Smith feels she is managing her symptoms effectively at this time and is aware of the Mental health services available to her, but she is not interested at this time.
- You will need to gather information from the participant/POA during the visit to document a plan.
- You will need to document this information in the PCSP, in the following questions: (“yes” must be selected for any participant with a BH diagnosis)
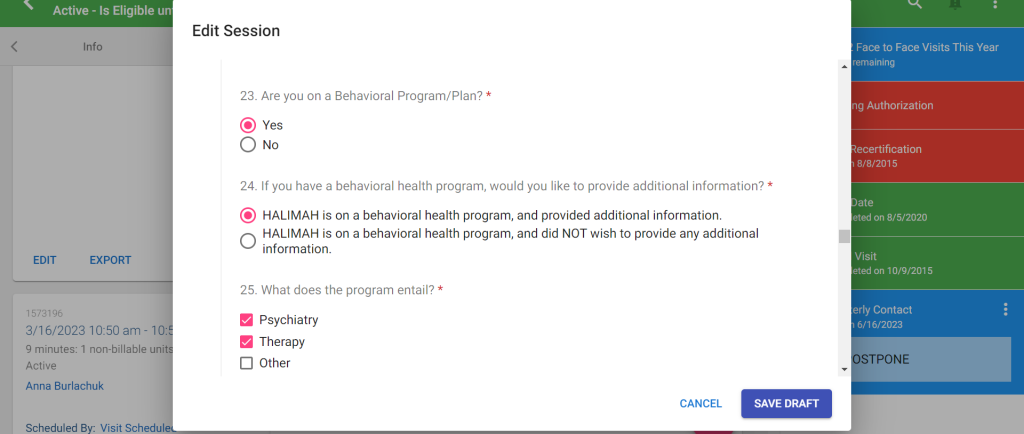


Writing that the Participant has Mental health Diagnosis and writing that there is no plan or indicating that the plan is not fully effective to meet the participants needs would not be considered sufficient.
If during the discussion of the Mental Health Plan with the participant, they express that they would like to attain Mental Health services (ie. Therapist, Psychiatrist, etc) then a Behavioral Health Referral can be done. The Service Coordinator will email their Supervisor with the participants name, the best phone number where providers for these services will be able to reach the participant, the Diagnosis that is related to the referral (ie. Depression, Anxiety, etc), what specific service they would like to be referred for and a small explanation of why the participant would like the service (ie. Therapy to help learn to manage Depression symptoms OR Psychiatry to discuss medications for Anxiety). The Supervisor will then ensure the referral to PA Health and Wellness is done and the specified Provider being requested will then reach out directly to the participant.
Employment and Benefits Counseling Guide
Employment Services
In the PCSP in Function Portal, there is a section that is specifically about employment/volunteering and we are responsible for ensuring that we are discussing services that are available to assist any participant with attaining or maintaining employment or volunteering.
We need to ensure that we are discussing available resources related to employment and documenting in our notes as well as in the PCSP what resources we have offered.
There are currently four types of employment services offered through CHC:
- Benefits counseling
- Job coaching
- Employment skills development
- Career assessment
Previously, prior to requesting employment services through CHC, referrals had to be done to OVR and WIPA to determine if they are able to provide the needed services. If referrals to OVR and WIPA are done and they are unable to begin services for the participant (ie. ptp is put on a wait list) then employment services can be requested through CHC. Referrals to OVR are no longer necessary prior to adding employment services to the participants’ care plan. However, depending on the situation there must still be a referral to WIPA (refer to the “who and what of employment services guide” below for additional details).
For a participant who does NOT want assistance with employment:
- No NEED, GOAL, or OUTCOME needed for Employment.
- PCSP must clearly state the reason why the participant does not want to pursue employment
For a participant who wants assistance with employment :
- Must have NEED, GOAL and OUTCOME related to finding employment
- Must also have Employment related Services listed in the Service plan
EXAMPLE IF PTP IS WORKING AND WANTS TO CONTINUE WORKING:
- Must have NEED, GOAL and OUTCOME related to maintaining employment
- Must also have Employment Services listed in Service plan
Providers outside of CHC:
- WIPA Hotline– 1-866-968-7842
- OVR (Office of Vocational Rehabilitation)
- PHILADELPHIA
- Vocational Rehabilitation Services
- 801 Market Street Suite 6034 Philadelphia, PA 19107
- 215-560-1900 Voice
- 800-442-6381* Voice
- Vocational Rehabilitation Services
- PITTSBURGH
- Vocational Rehabilitation Services
- 531 Penn Avenue Pittsburgh, PA 15222
- 412-392-4950 Voice
- 412-392-5921 TTY
- 800-442-6371* Voice
- 888-870-4474* TTY
- Vocational Rehabilitation Services
- PHILADELPHIA
Providers in Network
- Community Integrated Services, 215-238 7411
- If unsure of the provider the ptp would like to use TBD can be used
What is OVR?
The Office of Vocational Rehabilitation (OVR) serves people who have disabilities that present a substantial impediment to employment. Services are provided to individuals to prepare for, secure, retain, advance in or regain employment. OVR has 21 District Offices located around the state. Our counselors work every year with thousands of persons who have physical, mental or emotional disabilities.
Directory:
OVR Employment Service:
- https://www.dli.pa.gov/Individuals/Disability-Services/ovr/Pages/Individualized-Employment-Services.aspx
- Vocational Rehabilitation Home (pa.gov)
What is WIPA?
To amend the Social Security Act to expand the availability of health care coverage for working individuals with disabilities, to establish a Ticket to Work and Self-Sufficiency Program in the Social Security Administration to provide such individuals with meaningful opportunities to work, and for other purposes.
- provide in-depth counseling about benefits and the effect of work on those benefits;
- conduct outreach efforts to beneficiaries of SSI and SSDI (and their families) who are potentially eligible to participate in federal or state Work Incentives programs; and
- work in cooperation with federal, state and private agencies and nonprofit organizations that serve SSI and SSDI beneficiaries with disabilities.
WIPA Hotline– 1-866-968-7842 Monday through Friday from 8 a.m. – 8 p.m. ET.
Reminders:
- Employment can be added as a goal or added into a goal at any time without a full reassessment if the PCSP has been completed within last 365 days.
- Employment can be a standalone goal or connected to another goal.
- Employment goals can be short and long-term. Example: Jay would like to explore possibility of work when their chemo treatment is done. Goal would communicate need of finishing chemo with long-term goal of employment.
When does a participant need an Employment Goal?
- Participant expresses interest in work and/or exploration of the possibility
- Participant is actively seeking work – with or without support
- Participant is pursuing education (e.g. degree, certificate, credential)
- Referred (or self-referred) to any of the following:
- PA CareerLink®
- Work Incentives Planning and Assistance (WIPA) program
- PA Office of Vocational Rehabilitation (OVR)
- Any of the 5 Community HealthChoices HCBS Employment Services
- Ticket to Work (Employment Networks)
- Training Programs through Workforce Development (e.g., Energy Innovation Center)
- Other Employment Services including but not limited to grant-funded
- Receiving services from any of the organizations or services previously mentioned
- Participating in Pre-Apprenticeship or Apprenticeship program
- Participating in On-the-Job training (OJT) or other training program
- Participant is interested in finding another job – within current company or a different company
- Participant expresses need where participant agrees employment can help (e.g. socialization, housing stability, mobility)
- Participant is volunteering with plans to pursue employment
When is it helpful for a participant to have an Employment Goal or employment connected to another goal?
- When the participant is working and not receiving employment services of any kind, it is helpful to have maintenance of employment as either a standalone goal or connected within another goal. This shows the importance of employment in the participant’s life, as well as how it supports other goals for healthy living. It also allows a much quicker process if/when the participant needs additional help with employment quickly or suddenly (e.g. laid off, needs Employment service of some kind, redetermination).



Sorry, the comment form is closed at this time.